CRYSVITA® (burosumab-twza) is a fibroblast growth factor 23 (FGF23) blocking antibody indicated for the treatment of X-linked hypophosphatemia (XLH) in adult and pediatric patients 6 months of age and older.
ACCESS STEPS FOR CRYSVITA
The decision to prescribe CRYSVITA has been made. Now what?
Enroll your patient today! Kyowa Kirin Cares can help get your patient from prescription to treatment with an overview of insurance coverage, financial assistance options, and shipment coordination.
Step 1: Enrollment
Download the enrollment form, fill it out with your patient’s information, sign it, and fax it to 833-552-3299.

Provide complete and accurate information to reduce additional follow-up and potential treatment delay
- Completing confirmatory testing prior to submitting a completed enrollment form may prevent delays (and testing may be required by patient’s health plan).

Set expectations with your patient
- Patient consent is needed to facilitate Kyowa Kirin Cares access services and financial assistance options for those who qualify. If the patient or care partner wishes to consent, be sure to have them sign the Patient Authorization on the enrollment form
- Alternatively, a Case Manager can send the patient an enrollment form and assist them with the process over the phone
- Use the Patient Next Steps guide to help your patient understand the process and the role they play
Step 2: Authorization
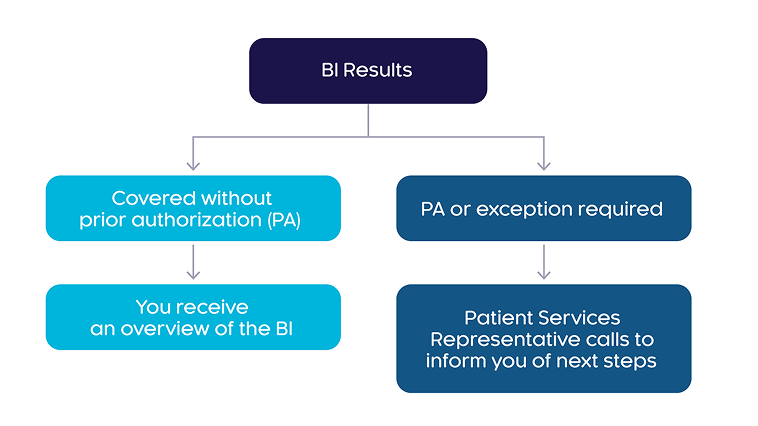
Upon receiving the completed enrollment form, Kyowa Kirin Cares will begin the benefits investigation (BI) process for the patient, then inform you of results within two business days.
 Show description
Show description
A flow diagram that shows 2 pathways for the benefits investigation results for the patient. In the first pathway, CRYSVITA is covered without prior authorization and you receive an overview of the benefits investigation. In the second pathway, prior authorization or exception is required for CRYSVITA and a Patient Services Representative calls to inform you of next steps.

A dedicated Case Manager will call the patient to review insurance coverage. They will inform the patient of the co-pay program and other assistance options.
Step 3: Procurement
A dedicated Patient Access Liaison (PAL) will work with you to coordinate a procurement option based on your patient’s BI results. CRYSVITA can be procured by an authorized Specialty Distributor or from a select group of Specialty Pharmacies, and ordering requirements may differ based on the patient’s coverage.
Questions? Ask a representative or call Kyowa Kirin Cares at 833-KK-CARES (833-552-2737) Monday through Friday, 8 am to 8 pm (ET).
Prior authorization and medical documentation for CRYSVITA
Understanding prior authorization
Documents and other criteria are commonly required by health plans to cover CRYSVITA. A dedicated Patient Access Liaison (PAL) will contact you with your patient’s plan-specific drug requirements.

Provide all documentation required by the patient’s health plan to prevent delays and denials
- Health plans may require documentation of past and current disease management interventions, such as use of supplement therapy or growth hormone, or orthopedic/dental surgery

Schedule testing
- Your patient’s health plan may have specific testing requirements
- A dedicated PAL can help you determine plan-specific criteria
- Timely submission of test results will facilitate the prior authorization (PA) process

Monitor communications with the patient’s health plan and answer any additional requests or questions promptly
Your patient’s plan may require genetic testing. A PAL can help you navigate diagnostic documentation and other plan requirements for your patient. Contact Kyowa Kirin Cares by calling 833-KK-CARES (833-552-2737).

Actor portrayal
Ready to start your patients on CRYSVITA?
Take the first step by filling out the enrollment form